Many tooth problems like extensive decay or impact injuries, can lead to infection or death of the nerve tissue inside a tooth. This can lead to various symptoms like severe pain, increased sensitivity, swelling of the gums, bad breath or tooth discoloration.
A root canal therapy, also called endodontic treatment, is a safe and straightforward procedure that treats the inside of the infected tooth, relieves pain and saves your natural tooth.
Gentle and Painless Endodontic Therapy
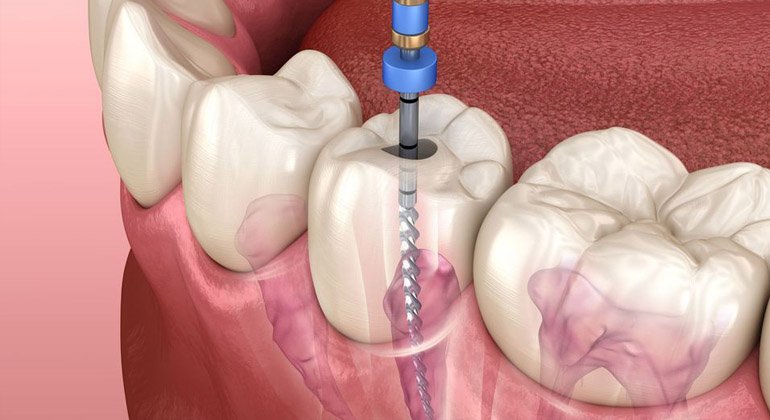
The pulp which contains nerves are central to a tooth. An infected or inflamed pulp is often the cause of pain. During a root canal treatment, our microscopic endodontist at the Özel Marmaris carefully removes the pulp inside the teeth, disinfects the root canals and places a filling to hermetically seal the space.
 Success rates for endodontic treatment are generally good. About 90 to 95 per cent of patients who undergo root canal treatment can expect a functional tooth after the treatment. The treated tooth should last a very long time, provided that you maintain good oral hygiene and generally look after your teeth. Of course, no therapy or replacement will last as well as a healthy tooth.
Success rates for endodontic treatment are generally good. About 90 to 95 per cent of patients who undergo root canal treatment can expect a functional tooth after the treatment. The treated tooth should last a very long time, provided that you maintain good oral hygiene and generally look after your teeth. Of course, no therapy or replacement will last as well as a healthy tooth.
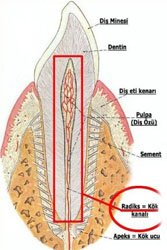
Tooth Anatomy Explained
A tooth is mainly made of a hard material called dentine. Enamel is the surface layer that protects the visible part of the tooth (crown). The part of the tooth that sits beneath the gumline is called the root. The root is the 'prong' that helps anchor the tooth into the jaw. Generally, front teeth have only one root, while molars have several. There may be several root canals in one root.
The hollow centre of a tooth is called the pulp chamber. This area contains the blood vessels, nerves and pulp. The pulp is a sensitive tissue that provides oxygen, nutrients and feeling to the tooth. The main function of the dental pulp is to regulate the growth and development of the tooth during childhood. The pulp extends from the roof of the pulp chamber down into the bottom of each root canal.
Once the tooth is fully formed, nutrition for the tooth comes from the tissues surrounding the root. Therefore, a tooth can function without its pulp and, in the majority of cases, can be kept indefinitely. After endodontic treatment, the tooth is 'pulpless', but it is not a dead tooth.
Symptoms of damage
- A diseased tooth pulp may cause inflammation or infection. The symptoms of a damaged or diseased tooth pulp may include:
- Unprovoked or spontaneous pain
- Sensitivity to hot and cold drinks and foods
- Pain when biting or chewing
- Loosening of the tooth
- Swelling of the gum near the affected tooth
- Oozing of pus surrounding the affected tooth
- Facial swelling
Sometimes, tooth pulp may become damaged or diseased without presenting any symptoms. In these cases, the problem is usually diagnosed by special tests or x-rays during a dental check-up or treatment for other dental concerns.
A range of causes
There are many events that can lead to disease or damage to dental pulp. Some of these include:- Deep-seated and untreated dental decay
- Decay beneath a deep filling
- Trauma that damages a tooth
- Habitual tooth grinding (bruxism)
- Advanced gum disease.
Research has also found a link between cigarette smoking and root canal treatment. A smoker is significantly more likely to need root canal treatment than a nonsmoker, but the reason for the higher risk is unclear.
Possible complications
If the infection is left untreated, complications could include:Spreading infection – once the pulp becomes infected, it loses its ability to fight the spread of the infection. If bacteria find their way into the pulp chamber, the bacteria will multiply unchecked. This can cause a severe infection or an endodontic abscess when it spreads into the surrounding bone (a pocket or 'blister' of pus).
 Localised bone loss – the infection may spread around the ends of the infected root canal and cause bone loss in the jaw.
Localised bone loss – the infection may spread around the ends of the infected root canal and cause bone loss in the jaw.Loss of tooth – the tooth may have to be removed, which interferes with the person's ability to bite and chew. Tooth replacements such as dentures, bridges and dental implants may not be possible or may not be tolerated. They may be more costly and involve other issues that also need to be considered.
Diagnosis
The dentist will listen to your symptoms, examine your teeth and other special investigations including taking x-rays. These x-rays also help the dentist to plan for the root canal treatment by revealing the number, size and curvature and depth of the roots. This will help to determine the complexity of the case.
Treatment
You may need one or more visits to complete the endodontic treatment, depending on the complexity of the root canals in your tooth. The exact procedure chosen by your dentist may differ from the procedure outlined here. Ask your dentist for further information.
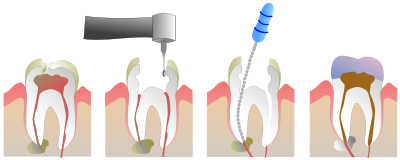
Generally, the typical root canal treatment includes:
- The procedure is usually performed using local anaesthetic. If the pulp is infected, anaesthesia may not always be necessary because the tooth no longer has any feeling.
- The affected tooth is wrapped in thin rubber (called a 'rubber dam') to prevent contamination of the root canals.
- The decayed portions of the tooth and any affected filling are removed.
- The pulp or pulp remnants are extracted.
- The dentist uses a special drill and small instruments to thoroughly clean and shape the root canals and to remove bacteria, pus and debris. The root canals may need to be shaped or hollowed out to ensure a smooth interior surface.
- The interior of the tooth is flushed with disinfectants and then dried.
- If the root canal is not infection free, it may be medicated and the tooth sealed with a temporary filling material. You may have to wait a few weeks, or even months, before the pulp canal is filled. If the dentist feels bacteria are still present at your next appointment, the cleaning procedure may be repeated and the tooth once again packed with medication. This stage will continue until the dentist feels the tooth is free from bacteria.
- The infection-free root canal is then sealed with long-lasting barrier materials (the root filling), usually a rubber-based material called 'gutta-percha'.
- The tooth then undergoes restoration and the biting surfaces need protection – an artificial biting surface for the tooth is fashioned out of regular filling material.
- In many cases, where there is considerable loss of the tooth structure, there may be a need for an artificial crown made from porcelain or gold alloy or other materials.
A normal tooth with a healthy pulp is yellowish-white in colour. A pulp-free tooth may, in time, turn grey. The dentist can advise you on appropriate aesthetic (cosmetic dentistry) procedures.

